Type 2 diabetes
“T2D is a Constant Condition in which the body does not use insulin properly or produce Sufficient Insulin to regulate blood Sugar levels“
Overview
Your body converts the food you eat into glucose (sugar) for energy. A hormone called insulin, produced by the pancreas, acts like a key, allowing this glucose to enter your cells. In type 2 diabetes, this process breaks down. Your cells become resistant to insulin, a condition known as insulin resistance. At first, your pancreas works overtime to produce more insulin, but eventually, it can’t keep up. This leads to high blood sugar levels, which can cause serious health problems over time.
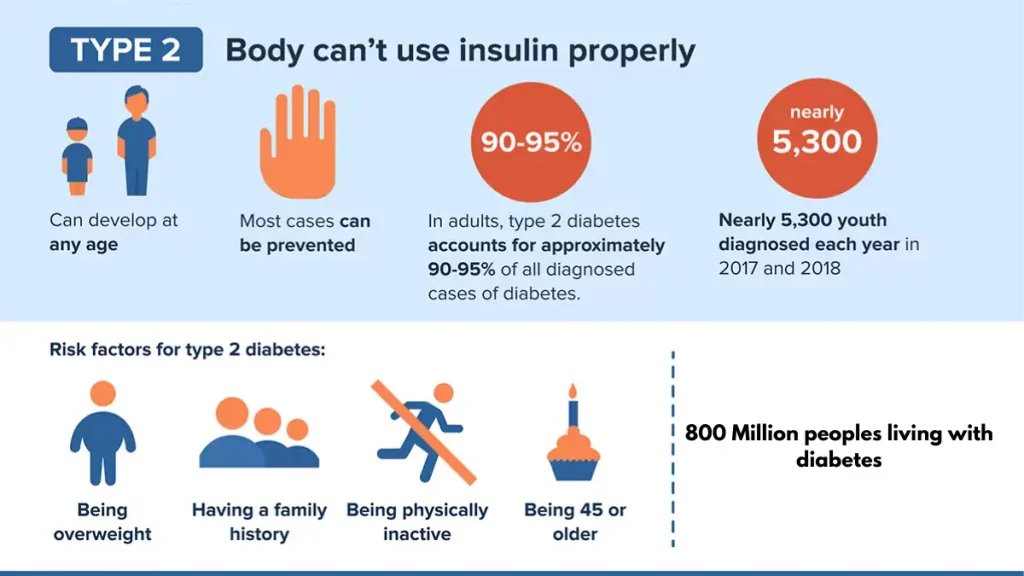
Type 2 diabetes occurs when the body is unable to use insulin properly, and sugar builds up in the blood. This is also called adult-onset diabetes. Over time, high blood sugar levels in diabetes can damage the eyes, kidneys, nerves, and heart. This is because the liver does not produce enough of the hormone insulin, which helps sugar enter cells. This also happens because the cells respond poorly to insulin by taking in less sugar. Both type 1 and type 2 diabetes can start in childhood and adolescence, but type 2 is more common in older adults, but the type 2 diabetes is becoming more common in young people.
There is no cure for type 2 diabetes, but losing weight, eating well, and exercising can help manage the condition. If we are not able to control our diet, exercise, and blood sugar, we may also need diabetes medications or insulin therapy. A healthy blood sugar (glucose) level is 70 to 99 milligrams per deciliter (mg/dL), if you have not been diagnosed with type 2 diabetes then yours is usually 126 mg/dL or higher. Type 2 diabetes is very common, with more than 38 million people in the United States (1 in 10 people) having diabetes, and about 90% to 95% of them have type 2 diabetes. Researchers estimate that it affects about 63% of the world’s population. It usually affects people aged 45 or older, but it can also affect people under the age of 45, including children. It is most often seen in middle-aged and older people.
If you have a family history of diabetes, you are more likely to have type 2 diabetes if you are overweight or obese. It is more common in people who are African American, Hispanic/Latino, American Indian, Asian American, or Pacific Islander.
Symptoms
Symptoms of type 2 diabetes often develop slowly over many years and may be so mild that you may not even notice them. Some people do not know they have the disease until diabetes causes health problems such as blindness or heart disease. When there are symptoms, they may include:

Detecting and treating diabetes can reduce the risk of developing diabetes complications. If you have any of these symptoms, a simple blood test can diagnose T2D
Cause
The leading cause of type 2 diabetes is insulin resistance. Insulin resistance occurs when muscle, fat, and liver cells don’t respond as they should to insulin, a hormone the pancreas makes that is essential for life and blood sugar regulation.
If your body isn’t responding correctly to insulin, your pancreas needs to make more insulin to try to control your blood glucose levels (hyperinsulinemia). If your cells become too resistant to insulin, your pancreas can’t make enough insulin, which can lead to type 2 diabetes.
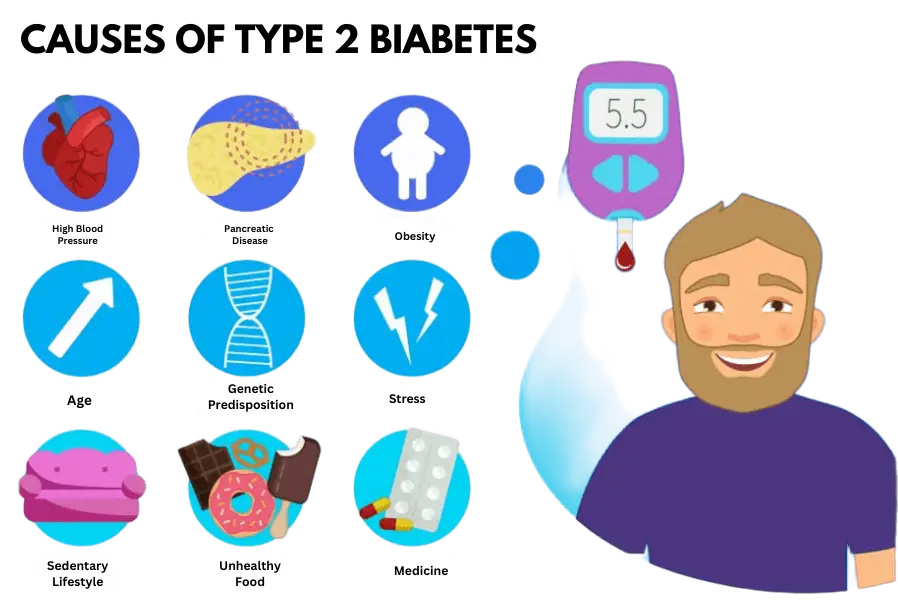
Muscle, fat, and liver cells don’t respond to insulin as they should, which results in the cells becoming quite restless, which means the pancreas, which makes insulin, can’t make enough to keep blood sugar levels within healthy limits. There are some risk factors:
People who smoke are 30% to 40% more likely to have type 2 diabetes than non smokers
Risk factors
Risk factors for diabetes depend on the type of diabetes, with family history playing a role in all kinds. Environmental factors and geography can increase your risk of type 1 diabetes. But race or ethnicity can also increase your risk of developing type 2 diabetes. However, it is not clear which groups including blacks, Hispanics, American Indians, and Asian Americans are at higher risk. Prediabetes Type 2 diabetes and gestational diabetes are more common in people who are overweight or obese, and the other types are listed below.
How Insulin Works
The role of glucose
Glucose is a sugar that is a source of energy for cells that build muscles and other tissues. Glucose comes from two primary sources: food and the liver. Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin. The liver stores it and makes glucose. When glucose levels are low, such as when you haven’t eaten for a while, the liver breaks down stored glycogen into glucose. This keeps your glucose levels within a normal range.
The exact cause of most types of diabetes is unknown. In all cases, sugar builds up in the bloodstream because the pancreas doesn’t produce enough insulin. Both types, type 1 and type 2 diabetes, are caused by a combination of genetic and environmental factors. This is unclear what those factors are.
Understanding and Avoiding Complications
Long-term complications of diabetes develop gradually. The less contained your blood sugar is, the higher your danger of complications. Eventually, more complications can be serious and even life-threatening. Pre-diabetes can lead to type 2 diabetes. Possible complications include:
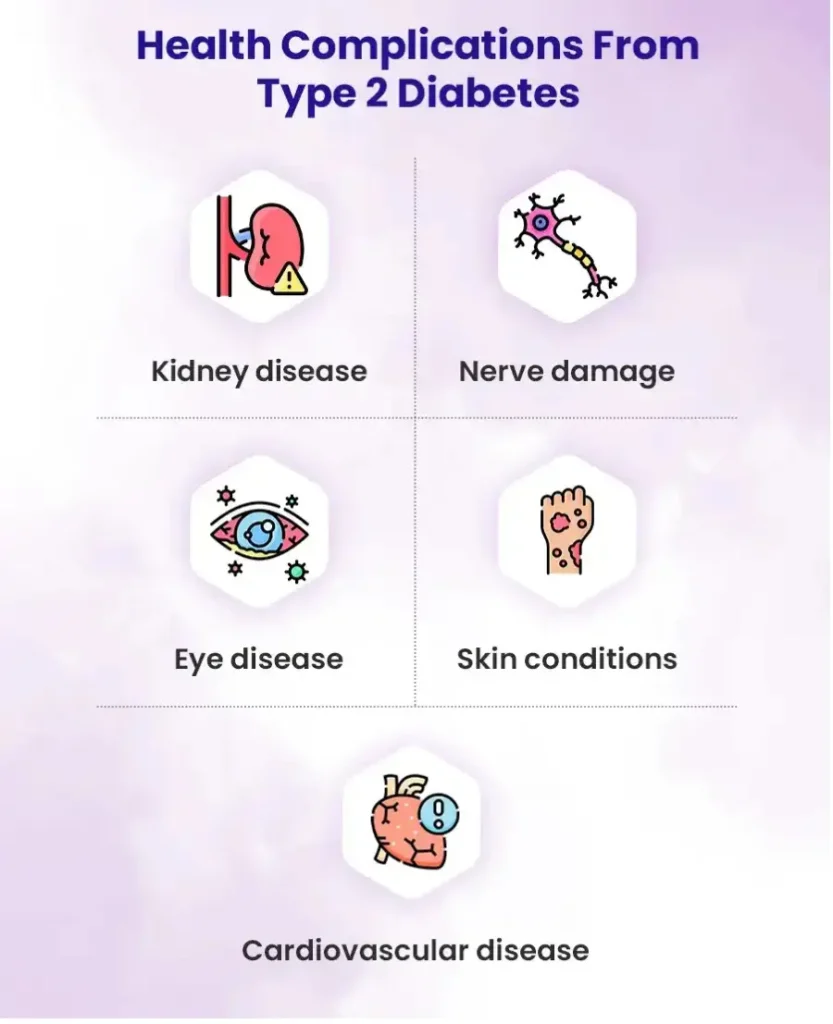
Uncontrolled high blood sugar can damage your body over time, leading to serious complications. Effective diabetes management is crucial for reducing your risk of:
- Cardiovascular Disease: Diabetes significantly increases the risk of heart attack, stroke, and high blood pressure.
- Kidney Disease (Nephropathy): High blood sugar can damage the delicate filtering system of your kidneys.
- Eye Damage (Retinopathy): Diabetes is a leading cause of blindness in adults.
- Foot Problems: Nerve damage and poor blood flow can lead to infections and, in severe cases, amputation.
Heart and blood vessel disease
Diabetes increases the risk of many heart problems, including chest pain (angina), heart attack, stroke, or narrowing of the arteries (atherosclerosis), including coronary artery disease. If you have diabetes, you are five times more likely to have heart disease or stroke, and it also increases the risk of a blood vessel in your heart or brain becoming fixed, putting you at risk of a heart attack, stroke, or heart failure
Nerve damage from Diabetes (Diabetic Neuropathy)
Eating too much sugar can damage the walls of the small bloods vessels that supply the nerves, especially in the legs. This can cause tingling, numbness, burning, or pain that usually starts in the fingers or toes and gradually spreads upward. Damage to the nerves related to the digestion can cause problems with diarrhea, nausea, vomiting, or constipation, which, for men, can lead to erectile dysfunction
Damage to the nerves related to the digestion can cause problems with diarrhea, nausea, vomiting, or constipation, which, for men, can lead to erectile dysfunction.
Skin and mouth conditions
Diabetes -up skin problems, which can also make bacterial and fungal infections
Error hearing
In people with diabetes, many problems of hearing are also common
Alzheimer’s disease
Type 2 can also increase the risk of diabetes dementia as Alzheimer’s Disease
Diabetes Related Depression
Symptoms of depression are also prevalent in people with type 1 and type 2 diabetes
Complications of gestational diabetes
Most women who have diabetes give birth to healthy children, but if blood sugar levels are not treated in a timely, it can cause problems for your children. Your baby may also have complications due to gestational diabetes, including:
How Is Type 2 Diabetes Diagnosed?
Test for Type one and Type two diabetes & prediabetes
A1C Test
Also called the hemoglobin A1C or HbA1c test, this is a simple blood test. The A1C test part your average blood sugar levels over the past 2 or 3 months.
Fasting Blood Sugar Test (FPG)
It measures your blood sugar after an overnight fast
Glucose Tolerance Test (OGTT)
These checks are usually done 1, 2 or possibly 3 hours after the check-up
Random Blood Sugar Test
How to Prevent Type 2 Diabetes
Lifestyle changes can help stop the onset of type 2 diabetes, the most common form of our disease. Making some lifestyle changes can also help you avert serious health complications of diabetes in the future, such as damage to the nerves, kidneys, and heart.
Treatments
Unlike many health conditions, you can reduce your risk of T2D diabetes by taking basic care of your health. It can include:
Exploring Your Treatment Options
The goal of type 2 diabetes symptoms and treatment is to manage your blood sugar levels to prevent complications. There is no one-size-fits-all approach; your plan will depend on your individual needs.
Lifestyle Changes
The cornerstone of diabetes management is adopting a healthy lifestyle. This includes a balanced diet, regular physical activity, and maintaining a healthy weight. For many, these changes alone can significantly improve blood sugar control.
Oral Medications
If lifestyle changes aren't enough, your doctor may prescribe medication. Metformin is often the first-line treatment. It works by reducing glucose production in the liver and improving your body's sensitivity to insulin. Other oral medications work in different ways to lower blood sugar.
Injectable Medications and Insulin
Some people with type 2 diabetes may need injectable medications, such as GLP-1 receptor agonists, which help the body produce more insulin after meals. Over time, as the pancreas produces less insulin, insulin therapy may become necessary to manage blood sugar levels effectively.
Blood Sugar Monitoring
There are many types of meters, but most of them work similarly. You can ask your care team or Doctor to show you how to do it, or you can do it yourself by reading the instructions on the box. And if you are sick and can't check your blood sugar yourself, you can have someone else use your meter to check your sugar. You can also use the method below to check your sugar and take steps to do so.
The Power of a Healthy Lifestyle
Your daily habits have a massive impact on diabetes management. Small, consistent changes can lead to big results.
Healthy Eating
There's no specific "diabetes diet," but the focus should be on balanced, nutritious meals.
- Prioritize whole foods like fruits, vegetables, whole grains, and lean proteins.
- Limit processed foods, sugary drinks, and refined carbohydrates.
- Practice portion control to help manage your weight and blood sugar.
A registered dietitian can help you create a personalized meal plan that you enjoy and can stick with.
Regular Physical Activity
Exercise makes your body more sensitive to insulin, helping you manage your blood sugar levels.
- Aim for at least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, swimming, or biking) per week.
- Incorporate strength training activities at least two days a week.
- Try to break up long periods of sitting by getting up and moving every 30 minutes.
Final Thoughts
Living with type 2 diabetes requires attention and care, but it doesn't have to control your life. By understanding the symptoms, working with your healthcare team, and embracing a healthy lifestyle, you can effectively manage your condition and reduce the risk of complications. Proactive health management is your best tool for living a long, healthy, and fulfilling life. Talk to your doctor today about your personal risk and the steps you can take to protect your health.
